What is Pancreatic Atrophy?
The atrophic pancreas is a non-specific condition that is common in elderly persons. Atrophy is a condition in which a body part loses some or all of its mass. This refers to the shrinkage of a cell, tissue, or organ. Atrophy is a physiological phenomenon that involves the reabsorption and disintegration of tissues through apoptosis. Atrophy is generally characterized by a decrease in cell size or number or both.
The permanent deterioration of the pancreas is known as an atrophic pancreas. This condition is linked to chronic pancreatitis. This condition is caused by pancreatic inflammation, which is largely caused by alcohol. This illness is characterized by persistent pancreatic inflammation. The organ’s typical structure and functioning are altered as a result of long-term inflammation. It is distinguished by irreversible pancreas damage caused by reversible alterations in acute pancreatitis. This condition can cause irreversible scarring and pancreatic impairment. Chronic pancreatitis that is not treated promptly leads to pancreatic atrophy, which is characterized by pancreatic shrinking.
The atrophic pancreas is rarely diagnosed in young people. Atrophy of the pancreas is non-specific and typical in elderly patients, however, in younger persons, it can be a sign of pathology. Most of the time, it is caused by old age, being overweight, or having end-stage chronic pancreatitis.
Pancreatic Atrophy Symptoms
This condition’s symptoms include upper abdominal pain, unexpected weight loss, and greasy-looking feces. Chronic pancreatitis is characterized by a decrease in digestive enzymes, resulting in stools that are oily and light in color. Other symptoms include:
- Breathing difficulty.
- Nausea and vomiting.
- Diabetes.
- decline in appetite.
- Feelings of being full.
Pancreatic Atrophy Causes
Pancreatic Atrophy is most common among the elderly, obese, and those with chronic pancreatitis. Pancreatic lipomatosis is a disorder in which fatty tissue grows in place of normal pancreatic tissue. Fat does not normally replace the entire pancreas, causing full shrinkage, but fat deposits dot the pancreas and cause deterioration.
The most prevalent causes of pancreatic atrophy in pediatric patients are cystic fibrosis, recurrent pancreatitis, and Pancreas Divisum. The most common thing that causes this disease is drinking alcohol. Among the additional reasons for this illness are:
- Autoimmune illnesses.
- Ischemia.
- Intraductal blockage
- Cystic fibrosis.
- Gallstones.
- a little infection
- A pancreatic injury.
- Hypercalcemia.
- A high lipid profile.
Pancreatic Atrophy Treatment
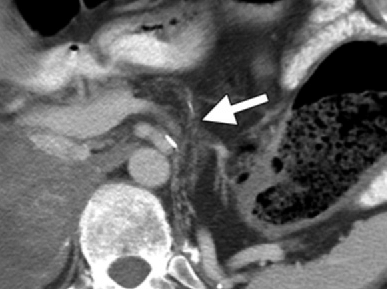
Pancreatic atrophy is commonly linked to chronic pancreatitis, which can be treated by alleviating associated symptoms like complications and pain and enhancing the body’s capacity to digest food. Atrophy and pancreatitis, for instance, can lead to the formation of pseudocysts, which in turn will need to be drained.
Chronic pancreatitis treatment can include pain management and resolving flare-ups. Treatment options often include anti-inflammatory and painkiller prescriptions. One method of pain management is an injection called a celiac plexus block, which stops pain signals from traveling from the pancreas to the brain.
When these treatments fail to provide relief, other surgical options include pancreaticojejunostomy, Whipple surgery, and total pancreatectomy with islet auto-transplantation. A pseudocyst can develop at the apex of the pancreas and grow in size, causing pain. Compression or cyst drainage are two options for treating this issue. Pancreatic cancer is more likely to strike those with chronic pancreatitis.
Pancreatic Atrophy Life Expectancy
Pancreatic atrophy is a natural consequence of aging, and by the time a person is 85 years old, their pancreatic weight can often drop from the typical range of 60–100 grams to 40 grams or less. This can make it easier to detect a small or mild pancreatic tumor, which can often appear more apparent on imaging examinations in comparison to the atrophied gland.
The damage to the pancreas is irreversible, but with adequate treatment, the patient can control a number of the symptoms. Medication, endoscopic procedures, or surgery are all possible forms of pancreatitis treatment. Type 3c diabetes develops in approximately one-third of those with chronic pancreatitis. This develops when pancreatic injury renders the organ incapable of secreting insulin. Chronic pancreatitis patients can sometimes develop fluid-filled sacs on the pancreas’s surface (pseudocysts). Chronic pancreatitis has a mortality rate that is higher than that of the general population; nonetheless, the 10-year survival rate following diagnosis is believed to be between 69 and 80 percent.
 Health & Care Information
Health & Care Information