Learn all about pseudothrombocytopenia definition, symptoms, causes and treatment.
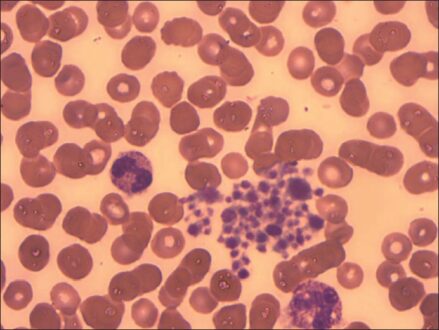
Pseudothrombocytopenia can occur in a number of settings, all of which can be identified by review of the peripheral blood smear and/or repeating the CBC using a non-EDTA anticoagulant.
Pseudothrombocytopenia is a diagnostic challenge for health-care providers and should be part of the early differential diagnosis in all cases of thrombocytopenia to avoid unnecessary tests and treatments.
Although seen in fewer than 2% of all cases of decreased platelets counts, some authors refer to pseudothrombocytopenia as the second most common cause of thrombocytopenia. PTCP has no clinical significance, but misdiagnosis may lead to unnecessary diagnostic tests and treatment.
The three different scenarios in which pseudothrombocytopenia can be seen are EDTA-induced platelet clumping, platelet satellitism, and giant platelet syndromes.3-5 in all three; the platelet count is falsely low because giant platelets and aggregates are not counted by the electronic particle counter. Several remedies have been proposed, such as warming the sample to 37°C or using additives or specific formulations of anticoagulants including buffered sodium citrate, heparin, ammonium oxalate, β-hydroxyethyltheophylline, sodium fluoride, CPT (trisodium citrate, pyridoxal 5′-phosphate and Tris), antiplatelet agents, potassium azide, amikacin, kanamycin or other aminoglycosides, and calcium replacement with the simultaneous addition of calcium chloride/heparin. According to available evidences, the most suitable and practical approach so far for most clinical laboratories seems, however, the recollection of blood samples using sodium citrate, CPT or calcium chloride/heparin as additives, maintaining the specimen at 37°C until the platelet count has been completed.
What is Pseudothrombocytopenia?
Pseudothrombocytopenia is an in vitro decrease in platelet count related to the ethylenediaminetetraacetate (EDTA)-dependent exposure, and should be considered in the differential diagnosis. It is mostly due to the presence of EDTA-dependent antiplatelet antibodies that recognize the platelet receptors GP IIb-IIIa, which are modified when calcium is chelated. This binding trigger platelet agglutination and clumping in vitro, which finally lead to a spuriously decreased platelet count reported by automated blood counters.
Pseudothrombocytopenia Definition
An inaccurately low estimate of the number of platelets in a sample of blood that is caused by clumping of the platelets in the laboratory sample rather than by a disease that affects platelet production or destruction is known as pseudothrombocytopenia.
Pseudothrombocytopenia Symptoms
Pseudothrombocytopenia symptoms vary with the time. You can bleed outside or inside your body. Sometimes it can be heavy or hard to stop. Some people get nosebleeds or bleeding gums.
You might also have:
- Blood in your urine or bowel movement
- Headaches
- Heavy menstrual periods
- Purple or red bruises, called purpura
- Tiny red or purple spots on your skin, called petechiae
- These symptoms might not start until your platelet count is very low.
Pseudothrombocytopenia Causes
The most common cause of pseudothrombocytopenia is a naturally occurring autoantibody against an epitope on GPIIb/IIIa that is exposed by the EDTA anticoagulant used for routine blood counts. In EDTA, these autoantibodies cause platelet clumping and falsely low platelet counts in vitro. Pseudothrombocytopenia may also result from in vitro platelet adherence (“satellitism”) to leukocytes, typically granulocytes, and a phenomenon that may also only occur in EDTA-anticoagulated blood. Either cause of pseudothrombocytopenia will be clearly demonstrated by examination of the peripheral blood smear. Other possible preanalytical factors to consider upon investigating platelet clumps include the collection method, that is, capillary venous or line draws. Capillary collections are prone to clotting and formation of platelet clumps. Viral infection, drugs, and medications, especially chemotherapeutic agents are all possible inducers of platelet clumping.
Pseudothrombocytopenia Treatment
Pseudothrombocytopenia treatments most important goal in clinical area is to get the right count of platelets. For the proper interpretation of laboratory values or results following points need to be carefully addressed:
- familial and personal history of diagnosed diseases
- Pharmacological history and treating the underlying cause of thrombocytopenia.
If your doctor can identify a condition or a medication that’s causing your thrombocytopenia, addressing that cause may clear up your thrombocytopenia. For example, if you have heparin-induced thrombocytopenia, your doctor will direct you to stop using heparin and prescribe a different blood-thinning drug. Your thrombocytopenia may persist for a week or more despite stopping all heparin therapy.
Blood or platelet transfusions, if your platelet level becomes too low, your doctor can replace lost blood with transfusions of packed red blood cells or platelets.
Medication, if your condition is related to an immune system problem, your doctor may prescribe drugs to boost your platelet count. The first-choice drug may be a corticosteroid. If that doesn’t work, he or she may try stronger medications to suppress your immune system.
Surgery, If other treatment options don’t help, your doctor may recommend surgery to remove your spleen (splenectomy).
Plasma exchange, Thrombotic thrombocytopenic purpura can result in a medical emergency requiring plasma exchange.
 Health & Care Information
Health & Care Information