Learn what is Paroxysmal Nocturnal Dyspnea (PND), its medical abbreviation, definition, symptoms, treatment, and causes.
Paroxysmal Nocturnal Dyspnea Defination
To define Paroxysmal Nocturnal Dyspnea pathology it is necessary to know the terms in detail. PND medical abbreviation stands for “Paroxysmal Nocturnal Dyspnea”. PND is also called alternatively called Paroxysmal Nocturnal Dyspnoea, Paroxysmal Dyspnea or Nocturnal Dyspnea. Let’s look at what is Paroxysmal Nocturnal Dyspnea defination:
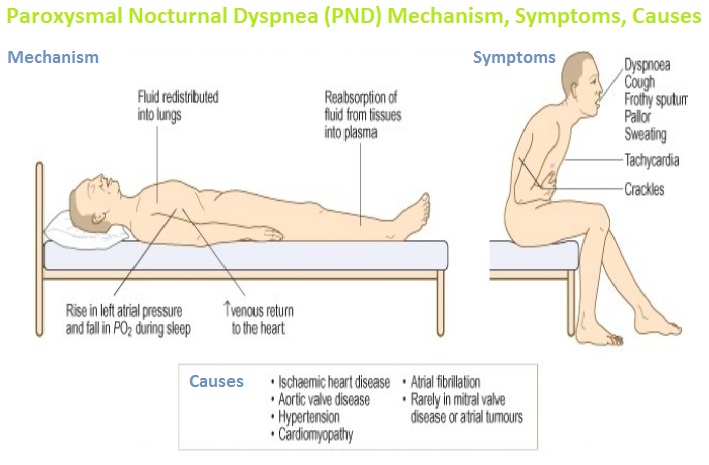
Paroxysmal Nocturnal Dyspnea is a medical condition that refers to the sudden attack of severe shortness of breath (suffocation) that awakens an individual from sleep. It normally happens in the first phase of the sleep cycle, with few hours of sleep (30 minutes to 2 hours), mostly in a reclining position.
Many things can wake you up during the night e.g. sound, movement, thirst, hunger, toilet run and nightmares. But there is nothing scarier than awakening from suffocation, choking, stifling and gasping for breath. In the event that you have never encountered this, you are fortunate. PND is a startling, fearsome and scary experience.
Imagine waking up all of a sudden from rest, gasping for air, coughing, wheezing and feeling like you are suffocating. Anxious and frightened, you may rapidly sit up and put your feet on the floor. The scientific term for this event is paroxysmal nocturnal dyspnea.
Cardiac Asthma and Paroxysmal nocturnal dyspnea (PND) are sometimes confused when PND is referred as cardiac asthma, as its signs and symptoms mimic those of the asthmatic attack. However, this is a misleading term. The two conditions are altogether different. The underlying pathology in asthma is a chronic inflammatory condition of airways in which the constriction of the airways occur leading to breathing difficulties while Paroxysmal nocturnal Dyspnea is due to the fluid buildup in lungs or pulmonary edema and is a sign of heart failure.
Paroxysmal Nocturnal Dyspnea Symptoms, Treatment, Causes
We have discussed Nocturnal Dyspnea Definition definition and nature. Let’s dig into more details of Paroxysmal Nocturnal Dyspnea, Paroxysmal Dyspnea, Nocturnal Dyspnea in the following:
What is Paroxysmal Nocturnal Dyspnea?
If we look at the pathology of Paroxysmal Nocturnal Dyspnea attacks or paroxysms. These are a sudden repetitions or intensifications of symptoms, for example, a pain, spasm, coughing, shaking and so forth.
Nocturnal means of or related to the night. It is the activity that happens or irritates amid night time. Dyspnea refers to the sensation of troublesome or uncomfortable breathing. It is a subjective experience perceived and reported by an affected person.
According to research paper published in National Center for Biotechnology Information, Paroxysmal Nocturnal Dyspnea is an intense form of Orthopnea. With the difference being that in Paroxysmal Nocturnal Dyspnea coughing and wheezing frequently persists while sitting in upright posture along the side of the bed with legs dangling. However, in Orthopnea this posture relieves the dyspnea.
Paroxysmal Nocturnal Dyspnea Causes
PND is brought on by the depression or despondency of the respiratory centers during rest, which may lessen arterial oxygen tension, especially in patients with interstitial lung diseases and decreased respiratory compliance.
The most widely recognized reason for PND is a failure of the left side of the heart in which legs may swell up with fluid accumulation. During the day, the fluid is retained in the legs. In night time, while sleeping, the fluid absorbs in the lungs especially in the air sacs bringing about an increment in total blood volume and blood pressure leading to pulmonary edema.
Following medical conditions are some of the Paroxysmal Nocturnal Dyspnea Causes:
- Chronic Obstructive Pulmonary Disease (COPD; a group of lung conditions including chronic bronchitis and emphysema that influences the lungs’ ability to perform its function normally)
- Cor pulmonale (an intense strain or hypertrophy [i.e. abnormal enlargement] as a result of diseases of the lungs or of other vessels)
- Heart failure (PND is the characteristic sign of Congestive Heart Failure)
- Obesity (does not specifically bring about difficulty in breathing while resting but rather regularly aggravates different conditions that leads to it)
- Panic disorders
- Sleep apnea
- Snoring
- Renal failure
- Cardiomyopathy
- Cardiac ischemia
- Cardiac valve diseases (mainly mitral valve)
Paroxysmal Nocturnal Dyspnea Symptoms
Paroxysmal Nocturnal Dyspnea Symptoms, sign and characteristics are given below:
- Acute shortness of breath while sleeping
- Coughing
- Wheezing
- Swelling in feet and ankles
- Elevated heart beats
- Cold sweats
- Fatigue
- Muscle weakness
- Edema
- Drowsiness
Paroxysmal Nocturnal Dyspnea Diagnosis Tests
Contingent upon symptomatic manifestations and pre-existing conditions, following Paroxysmal Nocturnal Dyspnea (PND) diagnosis tests may determine the exact reason for the onset of the symptoms:
- Chest X-rays
- ECG (electrocardiogram)
- Echocardiogram
- Pulmonary function tests
Paroxysmal Nocturnal Dyspnea Treatment
Instant approach to for Paroxysmal Nocturnal Dyspnea treatment and prevention are:
- Add more pillows during sleep to elevate upper body
- Stand upright and breathing when attack occurs
Paroxysmal Nocturnal Dyspnea treatment relies on the careful cause of the episode. Specialists by and large suggest weight reduction for obese patients, and supplemental oxygen may ease symptoms. On the off chance that the episodes are because of heart failure, steps are taken to treat fluid overload.
There are a few distinct ways in which PND can be addressed. The treatment ways adopted by doctor may incorporate a combination of:
- Heart medications
- Diuretics
- Bronchodilators
- Anti-hypertensive medications
- Oxygen therapy
- Vasodilator drugs
- Inotropic drugs
In some cases the doctor may advise to undergo a procedure called ultra-filtration to get rid of the excessive fluid in blood.
While experiencing treatment for PND the dietary regimen is modified for the most part. Consuming high amounts of salt regularly prompts a fluid over-burden and exacerbates breathing issues. In this manner, it is best to follow a diet low in sodium. Restrict the intake of:
- Sauces
- Condiments
- Fast food
- Frozen and canned food
- Processed foods
- Takeaway meals
Try to consume home-cooked meals as frequently as possible and substitute salt with healthy spices and herbs.
 Health & Care Information
Health & Care Information