Parasagittal Meningioma Meaning
Meningiomas result from spinal cord and brain membrane tumors. It can compress or pressure the nearby brain, nerves, and veins even though it is not technically a brain tumor. The most frequent head tumor is meningioma. Most meningiomas grow extremely slowly, sometimes going undetected for years. However, in some cases, they can cause permanent impairment by damaging adjacent brain tissue, nerves, or blood vessels.
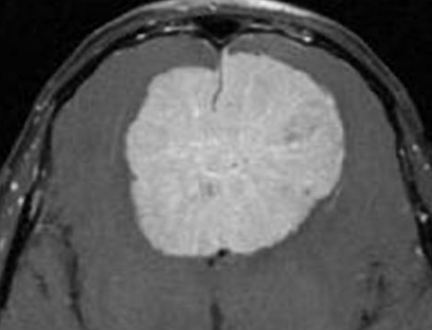
Meningiomas that extend into the superior sagittal sinus on at least one wall are known as parasagittal meningiomas.
There is a strong connection between the superior sagittal sinus and these types of tumors. This sinus is a huge venous canal that is situated in the middle of the two hemispheres of the brain. It receives the majority of the blood that is drained from the brain through the veins. Parasagittal meningiomas can invade this superior sagittal sinus partly or completely.
Parasagittal meningiomas have the potential to become enormously large and exert continuous stress on the underlying structure, which can result in brain swelling or edema. A tumor can occasionally penetrate the overlaying cranial bone, causing a bump to be felt beneath the scalp. Parasagittal meningiomas can arise anywhere along the superior sagittal sinus, including the frontal, parietal, and occipital lobes.
Parasagittal Meningioma Symptoms
The clinical manifestation of parasagittal meningiomas is dependent on their location along the sinus. Tumors near the central sulcus can cause sensory or motor seizures as well as contralateral hemiparesis/hemianesthesia. The following are some more symptoms:
- Headache: A new-onset headache that can be specific to the tumor’s site or diffuse due to elevated intracranial pressure.
- Seizures: Frontal tumors commonly cause motor or sensory focal seizures on the tumor’s contralateral side. When a tumor develops on the person’s dominant side of the brain, it can cause him/her to become unable to speak.
- Peripheral vision impairment.
Parasagittal Meningioma Causes
Meningiomas have an unknown etiology. The risk factors associated with the meningiomas are:
- Radiation exposure, particularly during childhood increases the likelihood of developing meningiomas.
- Neurofibromatosis type 2 increases meningioma risk.
Parasagittal Meningioma Treatment
Surgery is typically used to treat symptomatic parasagittal meningiomas. MRIs can be used to monitor and observe small to medium-sized incidental tumors that are not accompanied by brain edema. CyberKnife or Proton Beam radiation therapy can be used to treat small to medium-sized tumors in elderly patients with moderate symptoms and no significant mass effect.
Types of Surgical Procedures
- Surgery can easily reach parasagittal meningiomas because they are superficial. In the Meningioma Center, these tumors are surgically removed through the smallest possible skull bone opening (craniotomy) adjacent to the midline. The size and location of the tumor are taken into account when planning the craniotomy. A computer-assisted instrument that can locate the tumor and identify its anatomy directs the size of the craniotomy and tumor localization.
- Tumor resection is done with the help of a surgical microscope that magnifies the area so that the tumor can be lifted away from the brain. This is done by following the normal anatomical planes of dissection. By using this method, unnecessary trauma or injury to the brain’s tissue is prevented. An ultrasonic instrument is used to break up the tumor, reducing the pressure within the tumor and making it easier to remove.
- Opening the superior sagittal sinus is important to remove tumors that have grown into the sinus. This is executed by sinus repair. When the sinus is wholly obstructed pre-operatively, the entire sinus is resected. When there is a breakdown of the overlying cranial bone, the affected bone is removed and the cranial defect is fixed by a cranioplasty. Resection of the tumor’s meningeal origin is required for total tumor eradication.
 Health & Care Information
Health & Care Information