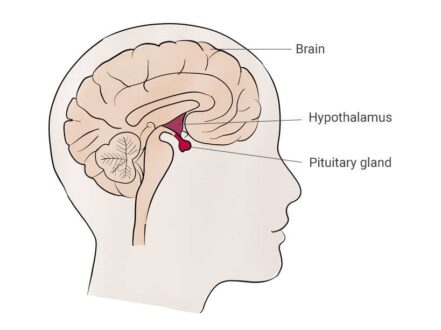
Learn all about panhypopituitarism prognosis, symptoms, causes and treatment options. The pituitary gland is called the master endocrine gland of the body because it controls the function of other endocrine organs.
The anterior pituitary produces the hormones thyrotropin (thyroid-stimulating hormone [TSH]), corticotropin (adrenocorticotropic hormone [ACTH]), luteinizing hormone (LH), follicle-stimulating hormone (FSH), growth hormone (GH), and prolactin (PRL). The anterior pituitary is controlled by specific hypothalamic-releasing hormones. The posterior pituitary produces vasopressin (antidiuretic hormone [ADH]) and oxytocin.
Panhypopituitarism is a condition of inadequate or absent production of the anterior pituitary hormones. Panhypopituitarism refers to involvement of all pituitary hormones; however, only 1 or more pituitary hormones are often involved, resulting in isolated or partial hypopituitarism. Some persons may have no symptoms or a gradual onset of symptoms. In other persons, the symptoms may be sudden and dramatic. The symptoms depend on the cause, rapidity of onset, and the hormone that is involved.
Severe head trauma, usually accompanied by coma or other neurologic problems, can also cause hypopituitarism. Approximately 15% of patients with a history of severe head trauma have been found to be GH deficient. Other hormone deficiencies may also occur after severe head trauma.
Acquired panhypopituitarism can occur as a result of tumors in the pituitary gland. It can also arise due to head injuries, radiation treatment, autoimmune conditions, stroke, brain infections, or brain surgery. If doctor suspects a pituitary disorder, he or she will likely order several tests to check levels of various hormones in your body. Your doctor may also want to check for hypopituitarism if you’ve had a recent head injury or radiation treatment that might have put you at risk of damage to your pituitary gland.
What is Panhypopituitarism?
Panhypopituitarism refers to loss of all pituitary function, both anterior and posterior pituitary function. However, some use this term to refer to loss of anterior pituitary function without diabetes insipidus (function of the posterior pituitary gland). Panhypopituitarism would involve loss to the pituitary hormones that control adrenal cortisol production, thyroid gland production, gonadal function (testosterone production in men, menstrual cycles in women and fertility in both men and women), growth hormone production, and in the case of loss of posterior pituitary function, diabetes insipidus resulting in frequent urination (particularly at night) and excessive thirst.
Panhypopituitarism Prognosis
Panhypopituitarism prognosis depends on the treatment. If hormone replacement therapy is adequate, the prognosis is good. Complications are often related to the underlying disease. You can expect a normal life span, as long as you regularly take the medications recommended by your doctor.
Panhypopituitarism Symptoms
Symptoms depend on which hormone or hormones are missing. Some of the symptoms are;
- Fatigue
- Weight loss
- Decreased sex drive
- Sensitivity to cold or difficulty staying warm
- Decreased appetite
- Facial puffiness
- Anemia
- Infertility
- Hot flashes, irregular or no periods, loss of pubic hair, and inability to produce milk for breast-feeding in women
- Decreased facial or body hair in men
- Short stature in children
Panhypopituitarism Causes
There are numerous causes of panhypopituitarism. The most common cause of panhypopituitarism is a pituitary tumor (also known as a pituitary adenoma0. Some other causes are;
- Infection
- Stroke
- Genetic factors
- Tumor on the pituitary gland
- Cancer that has spread
- Injury
- Trauma
- Cancer spread,
- Postpartum hemorrhage
- Brain surgery
- Radiation treatment
- Autoimmune inflammation (hypophysitis)
- Infections of the brain, such as meningitis
- Tuberculosis
- Infiltrative diseases, such as sarcoidosis, Langerhans cell histiocytosis and hemochromatosis
Panhypopituitarism Treatment
Panhypopituitarism treatment depends on the severity of disease. Oral replacement is usually with hydrocortisone, usually administered twice daily but can be administered 3 times daily. Prednisone may be considered advantageous because of twice-daily dosing (at about 20-25% of the dose for hydrocortisone). Treatment with the appropriate hormones is often the first step. These drugs are considered as “replacement,” rather than treatment, because the dosages are set to match the amounts that your body would normally manufacture if it didn’t have a pituitary problem. Treatment may be life-long.
Treatment for pituitary tumors may involve surgery to remove the growth. In some instances, doctors also recommend radiation treatment Levothyroxine (Levoxyl, Synthroid, others). This medication replaces deficient thyroid hormone levels caused by low or deficient TSH production.
- Sex hormones. These include testosterone in men and estrogen or a combination of estrogen and progesterone in women. Testosterone is administered through the skin with either a patch or a gel or by injection. Female hormone replacement can be administered with pills, gels or patches.
- Growth hormone. Also called somatotrophin, growth hormone is taken through an injection beneath your skin. It promotes growth, thus producing more normal height in children. Adults with a growth hormone deficiency also may benefit from growth hormone replacement, but they won’t grow taller.
 Health & Care Information
Health & Care Information