Learn all about metabolic encephalopathy symptoms, complications, causes and treatment options. There are two major types of metabolic encephalopathies, namely those due to lack of glucose, oxygen or metabolic cofactors (which are usually vitamin-derived) and those due to peripheral organ dysfunction. According to the National Institute of Neurological Disorders and Stroke, transmissible spongiform encephalopathy usually results in death within three months to a few years from the onset of the disease.
Metabolic encephalopathy is defined as a potentially reversible abnormality of brain function caused by processes of extra cerebral origin. These processes usually involve some metabolic upset (electrolytes, serum osmolarity, renal function or hepatic dysfunction), some deficiency (metabolic substrates, thyroid hormone, vitamin B12, etc.), some toxic exposure (drugs, alcohol, medicines, etc.) or systemic toxic states (sepsis, for example). Therefore, in metabolic encephalopathy, there is diffuse cerebral dysfunction. Of course, the degenerative diseases of the brain that result in dementia also produce diffuse dysfunction of the brain.
Other causes of metabolic encephalopathy include carbon monoxide or cyanide poisoning, which prevents hemoglobin from carrying oxygen in the bloodstream and results in tissue anoxia. In addition to liver and kidney waste products, it may include abnormally high or low blood sugar (hyperglycemia, hypoglycemia), thyroid problems, and sodium levels in the blood (hyponatremia=low sodium, hypernatremia=high sodium).
The metabolic encephalopathies comprise a series of neurological disorders not caused by primary structural abnormalities; rather, they result from systemic illness, such as diabetes, liver disease, renal failure and heart failure.
Metabolic encephalopathies usually develop acutely or subacutely and are reversible if the systemic disorder is treated. If left untreated, however, metabolic encephalopathies may result in secondary structural damage to the brain.
This can also include the presence of an infection in the body or presence of toxic chemicals. The encephalopathy usually resolves when the underlying chemical imbalance is restored or offending infection/toxin removed. Treatment may include medications to treat your symptoms and medications or surgery to treat the underlying cause.
What is Metabolic encephalopathy?
Metabolic encephalopathy is a transient or permanent impairment of brain function resulting from physiological insufficiency or aberrant metabolic processes accompanying certain systemic illness such as diabetes or liver disease.
Metabolic encephalopathy Symptoms
Symptoms of encephalopathy can be generalized causing decreased level of consciousness from minimal lethargy to coma. Encephalopathy can cause abnormal thought processes including confusion, poor memory, hallucinations, and even psychotic thinking.
- muscle weakness in one area
- poor decision-making or concentration
- involuntary twitching
- trembling
- difficulty speaking or swallowing
- seizures
- lethargy
- dementia
- tremors
- muscle twitching and myalgia
- Cheyne-Stokes respirations (an altered breathing pattern seen with brain damage and coma)
Metabolic encephalopathy Complications
Metabolic encephalopathy complications depend on the primary cause of encephalopathy and can be illustrated by citing a few examples from the wide variety of causes:
- Hepatic (liver) encephalopathy symptomized by brain swelling with herniation, coma, death.
- Metabolic encephalopathy irritability
- Anoxic encephalopathy wide range of complications, from none in short-term anoxia to personality changes, severe brain damage to death in long-term anoxic events).
- Uremic encephalopathy includes lethargy, hallucinations, stupor, muscle twitching, seizures and death.
- Hashimoto’s encephalopathy causes confusion, heat intolerance and dementia.
- Wernicke’s encephalopathy with complications as mental confusion, memory loss, decreased ability to move eyes.
- Bovine spongiform encephalopathy or “Mad Cow disease” with complications such as ataxia, dementia and myoclonus or muscle twitching without any rhythm or pattern.
- Shigella encephalopathy. Infectious causes of pediatric encephalopathy (irritability, poor feeding, hypotonia or floppy baby syndrome, seizures, death).
Metabolic encephalopathy Causes
The causes of encephalopathy are both numerous and varied. Some examples of causes of encephalopathy include:
- Infectious (bacteria, viruses, parasites, or prions)
- Anoxic (lack of oxygen to the brain, including traumatic causes)
- Alcoholic (alcohol toxicity)
- Hepatic (for example, liver failure or liver cancer)
- Uremic (renal or kidney failure)
- Metabolic diseases (hyper- or hypocalcemia, hypo- or hypernatremia, or hypo- or hyperglycemic)
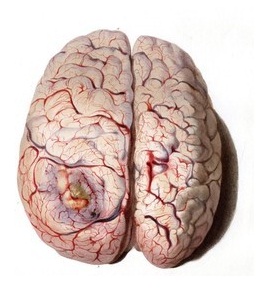
- Brain tumors
- Many types of toxic chemicals (mercury, lead, or ammonia)
- Alterations in pressure within the brain (often from bleeding, tumors, or abscesses)
- Poor nutrition (inadequate vitamin B1 intake or alcohol withdrawal)
- These examples do not cover all of the potential causes of encephalopathy but are listed to demonstrate the wide range of causes. Although numerous causes of encephalopathy are known, the majority of cases arise from several major categories (some examples in parentheses):
infection (HIV, Neisseria meningitides, herpes, and hepatitis B and hepatitis C)
brain anoxia or brain cell destruction (including trauma) - Some drugs may cause encephalopathy; for example, posterior reversible encephalopathy syndrome (PRES) may occur due to the use of drugs like tacrolimus and cyclosporine. This syndrome manifests with symptoms of headache, confusion, and seizures.
Metabolic encephalopathy Treatment
Metabolic encephalopathy treatment is directed toward reversal or control of the underlying process, supportive care, and prevention of complications such as infection, electrolyte imbalance, and cerebral edema. Successful treatment of metabolic encephalopathy depends upon early recognition of the symptoms and intervention to reverse the conditions that could lead to hypoxia or accumulation of toxins in the bloodstream. Delayed treatment could result in permanent or residual damage to the brain. Patients are maintained on a low-protein diet to lower blood ammonia levels since ammonia is a by-product of protein metabolism. Comatose patients may require special tube feedings and life support systems. Liver transplantation may be considered in patients with chronic liver cirrhosis.
 Health & Care Information
Health & Care Information