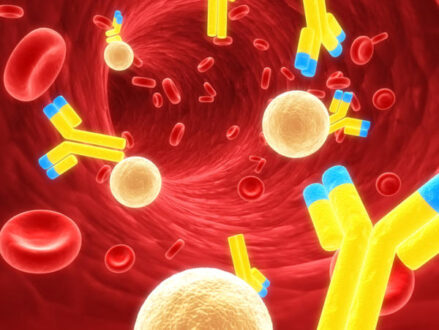
Learn all about Hypogammaglobulinemia symptoms and causes. Hypogammaglobulinemia, also known as Common Variable Immunodeficiency (CVID), is a disorder that falls into the category of the primary immunodeficiency diseases, meaning its main debilitating effect on the body is a weakening of the immune system that makes the individual susceptible to higher rates of infection and illness, among other symptoms. CVID is caused by a lack of B-lymphocytes, which results in low levels of immunoglobins (or antibodies), hence the effect on the immune system’s functionality.
Hypogammaglobulinemia, decreased antibody production in response to antigenic challenge, and recurrent pyogenic infections, often associated with hematologic and autoimmune disorders. Most patients have normal numbers of circulating B cells but lack plasma cells and appear to have an intrinsic defect of B cell differentiation. However, two other forms are also recognized: that due to a disorder of T lymphocyte regulation and that due to production of autoantibodies against T and B lymphocytes.
Hypogammaglobulinemia results from a decrease in the manufacture of white blood cells and immunoglobulins in the body system. It can also be caused by secondary factors. Diagnosis of hypogammaglobulinemia starts with a physical test and evaluation of the patient’s family medical history. Normally, the physical assessment is standard for individuals having agammaglobulinemia. Examination is an important aspect of the diagnosis of hypogammaglobulinemia. Some of the tests that are carried out during the assessment of agammaglobulinemia are serum IgM test, serum IgA test, and serum IgG test and serum immunoelectrophoresis.
A positive family history may suggest the diagnosis and guide testing, but a negative family history does not exclude X-linked agammaglobulinemia (Bruton agammaglobulinemia; XLA), as new mutations may constitute more than half of the cases in some series.
Duloxetine, Sertraline and Paroxetine can be used as medications. Before the start of hypogammaglobulinemia treatment, the health care provider should consider the dangers and advantages of administering any medications that can reduce the level of antibodies in the patient’s bloodstream.
What is Hypogammaglobulinemia
Hypogammaglobulinemia is a medical condition with elevated levels of gamma globulin. It is a type of immunoproliferative disorder. Hypogammaglobulinemia is an immune disorder characterized by a reduction in all types of gamma globulins, including antibodies that help fight infection. It may be congenital (present at birth), related to medication; it may be due to a kidney or gastrointestinal condition, cancer or severe burns.
Hypogammaglobulinemia Symptoms
Hypogammaglobulinemia have many symptoms. Some of them are listed below;
• Fatigue
• Handicap/Disability Parking Permit Levothyroxine Naltrexone
• Pain
• Anxious mood
• Insomnia
• Depression
• infections of the respiratory tract
• Infections of the skin
• Sinusitis
• Pneumonic infections
• Infections of the middle ear (otitis media)
• Infection of the eye (conjunctivitis)
• Diarrhea
• Bronchitis
• Growth retardation
• Abnormalities of lymphoid tissue and organs.
• Developmental abnormalities (e.g., of skeleton or chest wall)
• Abnormalities of skin and mucous membranes (e.g., scars, rash, or livedo reticularis)
• Ear, nose, and throat abnormalities
• Pulmonary abnormalities (e.g., bronchiectasis and lung fibrosis with rales, rhonchi, and wheezing)
• Cardiovascular abnormalities (e.g., a loud pulmonic heart sound, right ventricular heave, and tricuspid regurgitation murmur suggesting pulmonary hypertension; jugular venous distention, tender hepatomegaly, and lower-extremity edema suggesting cor pulmonale)
• Neurologic abnormalities (e.g., paralytic poliomyelitis or deep sensory loss with decreased vibratory and position sense of limb segments)
Hypogammaglobulinemia Cancer
Hypogammaglobulinemia is a disorder in which the body makes low amounts of infection-fighting antibodies (also known as gamma globulins). This leaves the person susceptible to infections. About 5% to 10% of thymoma patients develop hypogammaglobulinemia. About 10% of patients with hypogammaglobulinemia have a thymoma. Removing the thymus does not help correct this disease.
Hypogammaglobulinemia Prognosis
Prognosis depends on the course of the underlying disease. Hypogammaglobulinemia can sometimes be resolved by addressing the underlying condition. Prognosis has improved significantly since the introduction of IVIG therapy to routine practice. The prognosis largely depends on whether there is severe autoimmune disease; whether there are recurrent infections that cause structural lung damage; and the development of a malignancy (cancer). Other major factors that influence prognosis include the extent of end-organ damage and how successfully infections can be prevented.
Hypogammaglobulinemia Life expectancy
The life expectancy of CVID patients has considerably improved over the past 30 years from initially 12 years to currently over 50 years. Reduced survival was significantly associated with age at diagnosis, lower baseline IgG, higher IgM and fewer peripheral B cells. The risk of death was 11 times higher for patients with non-infectious complications such as lymphoma, chronic hepatitis, structural lung disease and chronic gastrointestinal disease.
 Health & Care Information
Health & Care Information