Erythroblastosis Fetalis definition, causes, symptoms, prevention, diagnosis, and treatment. It is a blood disorder that occurs when the blood types of a mother and baby are incompatible. It is also called as hemolytic disease of the newborn (HDN).
Erythroblastosis Fetalis is relatively uncommon in the United States due to advances in early detection and treatment, limiting it to approximately 4,000 cases a year. It is more likely to happen during a mother’s second or subsequent pregnancy.
Rh incompatibility and ABO incompatibility are two major causes of erythroblastosis fetalis. Erythroblastosis Fetalis due to Rh incompatibility occurs more frequently and is often called Rh disease; it is about three times more likely in Caucasian babies than in African-American babies. Erythroblastosis Fetalis can be treated during pregnancy or after the baby is born.
Erythroblastosis Fetalis treatment was first identified in 1932 at Boston Children’s Hospital by Dr. Louis Diamond. He went on to develop the first successful treatment for Erythroblastosis Fetalis through transfusion procedure, in the 1940s.
Erythroblastosis Fetalis Definition
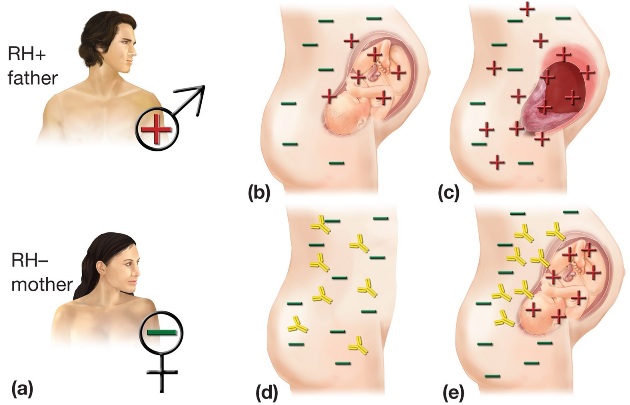
Erythroblastosis Fetalis is a hemolytic disease of the newborn (HDN) that occurs when the system of a Rh- mother produces antibodies to an antigen in the blood of a Rh+ fetus. here is how to medically define Erythroblastosis Fetalis:
Erythroblastosis Fetalis is a hemolytic disease of the newborn, characterized by an increase in circulating erythroblasts and jaundice, that occurs when the immune system of a Rh-negative mother produces antibodies to an antigen in the blood of a Rh-positive fetus, which crosses the placenta and destroys fetal red blood cells.
Erythroblastosis Fetalis Prevention, Treatment, Causes, Symptoms
Let’s look at the erythroblastosis fetalis prevention, causes, symptoms, diagnosis, and treatment in detail:
What Causes Hemolytic Disease of the Newborn (HDN)?
Erythroblastosis Fetalis or Hemolytic Disease of the Newborn is caused when the blood types of a mother and baby are incompatible. If the baby’s incompatible red blood cells cross over to his mother, through the placenta during pregnancy or at delivery, her immune system sees them as foreign and responds by developing proteins called antibodies to attack and break them down. This can lead to several complications that range from mild to very severe.
The mother’s immune system also keeps these antibodies in case the incompatible red blood cells appear again, making her “sensitized.” Because of this, Erythroblastosis Fetalis is more likely to occur during a mother’s second or subsequent pregnancy, or following a miscarriage or abortion.
A person’s blood type is determined by the presence of two different types of proteins, called antigens. The A, B and O antigens represent the classification of a person’s blood as Type A, B, AB or O. If a person also has the Rh factor antigen, his blood is Rh -positive, and if not, it is Rh-negative.
Rh Incompatibility
Erythroblastosis Fetalis most frequently occurs when a mother with Rh-negative blood becomes pregnant by a Rh-positive father, resulting in a Rh-positive baby. This type of Erythroblastosis Fetalis is often called Rh disease.
ABO Incompatibility
Although it is not as common, Erythroblastosis Fetalis can also occur when a mother and baby have incompatible blood types, specifically:
| Mother blood type | O | A | B |
| Baby blood type | A or B | B | A |
Erythroblastosis Fetalis Symptoms
The most common symptoms of Erythroblastosis Fetalis are:
- pale skin
- yellowing of the amniotic fluid, umbilical cord, skin, and eyes
- enlarged liver or spleen
- severe swelling of the body
Complications of Erythroblastosis Fetalis during pregnancy:
- Mild anemia: When the baby’s red blood cell count is deficient, his blood cannot carry
enough oxygen from the lungs to all parts of his body, causing his organs and
tissues to struggle. - Hyperbilirubinemia and jaundice: The breakdown of red blood cells produces bilirubin, a
brownish yellow substance that is difficult for a baby to discharge and can build up in his blood (hyperbilirubinemia) and make his skin appear yellow. - Severe anemia with enlargement of the liver and spleen: The baby’s body tries to compensate for the breakdown of red blood cells by making more of them very quickly in the liver and spleen, which causes the organs to get bigger. These new red blood cells are often immature and unable to function completely, leading to severe anemia.
- Hydrops fetalis (fetal hydrops): When the baby’s body cannot cope with the anemia, his heart begins to fail and large amounts of fluid buildup in his tissues and organs.
Complications of Erythroblastosis Fetalis after birth:
- Severe hyperbilirubinemia and jaundice: Excessive buildup of bilirubin in the baby’s
blood causes his liver to become enlarged. - Kernicterus: Buildup of bilirubin in the blood is so high that it spills over into
the brain, which can lead to permanent brain damage.
Erythroblastosis Fetalis Prevention
Erythroblastosis Fetalis is very preventable. Erythroblastosis Fetalis prevention is easy. Today, nearly all women with Rh-negative blood are identified in early pregnancy through blood tests. If a mother is Rh-negative and has not been sensitized, she is usually given a drug called Rh immunoglobulin, or RhoGAM. This specially developed blood product prevents a Rh-negative mother’s antibodies from reacting to her baby’s Rh-positive red blood cells. Mothers are typically given RhoGAM around the 28th week of pregnancy and again within 72 hours of giving birth.
Erythroblastosis Fetalis Diagnosis
Erythroblastosis Fetalis can be diagnosed during pregnancy or after the baby is born. Tests conducted during pregnancy may include:
- complete blood count test for the mother
- ultrasound
- amniocentesis
- cordocentesis
After birth, tests may include:
- complete blood count test for the baby
- umbilical cord blood test
Erythroblastosis Fetalis Treatment
Erythroblastosis Fetalis can be treated during pregnancy or after the baby is born. Treatment during
pregnancy may include:
- blood transfusion
- early delivery of the baby if severe complications arise and baby’s lungs are mature
After birth, treatment may include:
- blood transfusion
- intravenous fluids
- oxygen or mechanical breathing machine
- exchange transfusion to replace the baby’s damaged blood with fresh blood
 Health & Care Information
Health & Care Information