Learn all about dysgerminoma symptoms, causes, treatment, prognosis and tumor markers
Dysgerminomas occur most often in the ovaries, but they may also occur in other areas of the body, including the central nervous system. Some dysgerminomas make a hormone called beta-human chorionic gonadotropin (beta-HCG) that may cause signs and symptoms of disease.
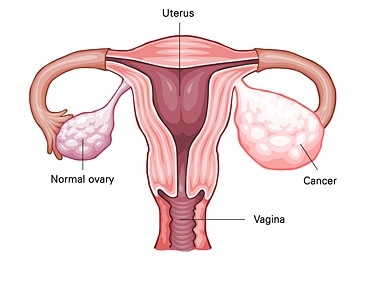
It is a type of cancer that begins in germ cells in females. Germ cells are cells that form sperm in males or eggs in females. Dysgerminomas tend to grow and spread slowly. They are the most common type of ovarian germ cell tumor. They usually occur in teenage girls or young women.
Abdominal symptoms including pressure, pain, pelvic pressure, low back discomfort, mild nausea, feeling full early when eating, constipation and gas are all non-specific in nature. In their early manifestations they are asymptomatic.
The incidence of dysgerminomas has remained unchanged over the last 30 years. The frequencies of the most common malignant ovarian neoplasms in women of reproductive age are as follows: epithelial tumors (42%); dysgerminoma and other germ cell tumors (GCTs) (30%); metastatic Krukenberg tumors (14%); and sex cord stromal tumors (ie, Sertoli-Leydig cell tumors) (13%).
What is Dysgerminoma?
Dysgerminoma is the most frequent malignant germ cell tumor of the ovary. Dysgerminomas are generally solid and large with a white surface and are plain or irregular. When dissected, they look white and homogeneous and sometimes have necrotic areas.
Dysgerminoma Symptoms
Dysgerminoma are almost totally symptoms free or asymptomatic in the early stages. Abnormal bleeding during menstruation should raise alarm and suspicion but again non-specific. The symptoms can be summarized as:
- Asymptomatic in early stages of growth and development
- Pelvic pain
- Excessive and abnormal bleeding during menstruation
- Dysuria
- Increased frequency of urination
- Mild abdominal symptoms
- Pelvic mass or Pelvic fullness
Dysgerminoma Causes
The exact cause of Ovarian Dysgerminoma is unknown; however they are thought to occur if the Germ
Cells that escape encapsulation from the Ovarian Follicle fail to die. The other causes include:
- Genetic defects like presence Y chromosome in females or presence of isochromosome 12p, amplification in the region of short arm of chromosome 12 and mutations in the exon 17 of CD117
- Individuals with the family history of ovarian cancers are at increased risk of Dysgerminoma of the Ovary
- Radiation exposure
- Chemical exposure
- Certain food
- Foreign body
- Pesticides
- Exposure to carcinogens in cigarette smoke
- Prior history of Chemotherapy for different malignancy.
Dysgerminoma Treatment
Dysgerminoma treatment is of various types. These tumors are highly treatable and respond well to chemotherapy and radiation particularly when these treatments are done together (chemotherapy can shrink the tumor, but it is recommended that radiation be given to the patient, as well). The tumor may metastasize, or spread, to the liver, lungs, lymph nodes, or bones. Women with stage I dysgerminoma often undergo surgery that isolates the mass as much as possible in order to preserve their fertility. This procedure, along with aggressive follow-up care, improves their prognosis considerable. There are different types of treatment for patients with ovarian germ cell tumors.
Four types of standard treatment are used:
- Surgery
- Observation
- Chemotherapy
- Radiation therapy
New types of treatment are being tested in clinical trials.
- High-dose chemotherapy with bone marrow transplant
- Follow-up tests may be needed.
- Unilateral salpingo-oophorectomy: A surgical procedure to remove one ovary and one fallopian tube.
- Total hysterectomy: A surgical procedure to remove the uterus, including the cervix. If the uterus and cervix are taken out through the vagina, the operation is called a vaginal hysterectomy. If the uterus and cervix are taken out through a large incision (cut) in the abdomen, the operation is called a total abdominal hysterectomy. If the uterus and cervix are taken out through a small incision (cut) in the abdomen using a laparoscope, the operation is called a total laparoscopic hysterectomy.
- Bilateral salpingo-oophorectomy: A surgical procedure to remove both ovaries and both fallopian tubes.
- Tumor debulking: A surgical procedure in which as much of the tumor as possible is removed. Some tumors cannot be completely removed.
Dysgerminoma Prognosis
Dysgerminoma prognosis of 5-year is 96% if the tumor is confined to the ovary and 63% if extension occurs beyond the ovaries. Pregnancy does not alter the prognosis of most ovarian malignancies, but complications such as torsion and rupture may increase the incidence of spontaneous abortion or preterm delivery. Prognosis of dysgerminoma depends on;
- The stage of the tumor
- The type of tumor
- The size of the tumor
- Age of the individual
- Overall health of the individual
- Tumor stage at detection
- Location of tumor
- Number of masses of tumors within the ovary
- Presence of metastasis and the organs involved with metastasis
- Its ki-67 value – a protein found in cells that is a good indicator of how fast the tumor cells are growing. The ki-67 value is determined by a pathologist and is usually mentioned in the pathology report
- Patient’s response to treatment such as chemotherapy
- Patient’s response to treatment such as radiation therapy
Dysgerminoma Tumor Markers
Dysgerminoma tumor markers are useful for their workup. Therefore, useful tumor markers for the workup of dysgerminomas include the following:
- Beta-hCG
- AFP
- LDH
- Serum lactic dehydrogenase
- Inhibin A and B
- Cancer antigen 125 (CA-125) – For epithelial tumors
 Health & Care Information
Health & Care Information