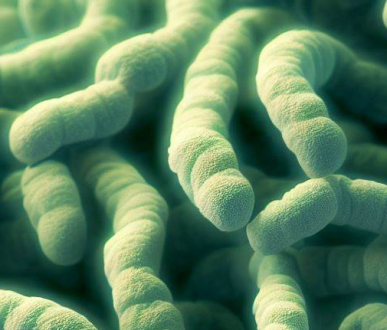
The bacteria Clostridium ramosum is anaerobic, has a Gram-positive morphology, is non-motile, and produces spores. C. ramosum was formerly classified to the genus Erysipelatoclostridium exclusively based on ribosomal protein-based phylogenetic trees.
C. ramosum is found in human intestinal commensal flora and is typically isolated from infant stool. C. ramosum is part of the normal intestinal flora and is rarely found to be an infectious disease-causing agent when it is separated from clinical samples.
Patients that have C. ramosum bacteremia tend to be older, immunocompromised, suffer from a likely gastrointestinal cause, and possess a higher fatality rate. In immunocompromised hosts, C. ramosum bacteremia requires careful assessment and treatment.
Clostridium Ramosum Susceptibility
Anaerobic Clostridium Ramosum resists various antimicrobials. Metronidazole, Chloramphenicol, Vancomycin, Carbenicillin, and Penicillin are all effective against all strains of bacteria when blood levels are easily achievable.
C. ramosum is highly susceptible to the following:
- Piperacillin-tazobactam.
- Amoxicillin/clavulanate.
- Ampicillin/sulbactam.
- Imipenem.
- Meropenem.
- Metronidazole.
- Vancomycin.
- Chloramphenicol.
Some types of C. ramosum produce β-lactamases that make them less sensitive to penicillin and cephalosporins.
Clostridium Ramosum Sensitivities
Clostridium Ramosum is a bacterium or a microbe that is typically found in the human gut but can also be found in other regions of the body. It belongs to the bacterial class Clostridia. C. ramosum is a bacillus-shaped bacterium that does not require oxygen for survival.
C. ramosum is rarely recognized as the major cause of infection, hence its pathogenicity is greatly underestimated. C. ramosum infections are most common in immunocompromised elderly people and small children under five with inner ear infections. Occasionally, C. ramosum infects healthy people. Infections like these are typically opportunistic and develop in specific situations, such as after trauma or surgery, or when there are other underlying medical disorders present.
The following are some methods for identifying the sensitivities of Clostridium Ramosum:
Laboratory Methods
Researchers use microbial culture and genetic sequencing, among other lab techniques, to examine Clostridium ramosum’s sensitivity. These techniques reveal its responses to various stimuli and aid in the interpretation of its potential effects.
Bioinformatics Approaches
When it comes to understanding the sensitivity of Clostridium ramosum on a molecular level, the tools of bioinformatics play an essential part. Understanding its genetic makeup and functional capacities is greatly aided by high-throughput sequencing data.
Clostridium Ramosum Gram Stain
The Gram stain is one of the longest-standing methods used to identify bacteria in the laboratory. As cultures mature, cell wall alterations associated with loss of viability allow certain gram-positive species to stain gram-negative or gram-variable. Clostridium species are usually anaerobic, endospore-forming, and gram-positive rods, but others are stained gram-negative or gram-variable and their spores are hard to identify.
C. ramosum’s Gram stain variability, lack of spores, and peculiar clostridial morphology make it hard to identify in the lab. The loss of gram-positive morphology is believed to occur primarily in direct stains of clinical samples, in cultures after prolonged incubation, or in species presenting terminal spores. As a result, C. ramosum can be misinterpreted as belonging to other genera, and the number of positive cultures is likely underestimated.
Clostridium Ramosum ICD-10
The ICD-10 system is used by doctors to categorize and code all procedures, diagnoses, and symptoms to process insurance claims. The WHO (World Health Organization) played a significant role in its creation.
There is no particular ICD-10-CM diagnostic code for Clostridium ramosum. However, for the sake of insurance reimbursement, several other codes can be used to denote the diagnosis such as:
B96.7: Clostridium perfringens-related illnesses categorized elsewhere.
B96.89: Other specific bacterial agents that cause diseases, and are listed elsewhere.
A41.4: Sepsis brought on by anaerobes, including some Clostridium species.
R78.81: Bacteremia, which can be brought on by a variety of Clostridium species.
 Health & Care Information
Health & Care Information