The thick layer of blood vessels and pigmented cells that cover the back of the eyeball, dividing it into two halves, is known as the choroid. To put it another way, it resembles the body of a wine glass because it is one of three parts of the uveal tract. There are three levels to it, and diseases can attack any one of them. It consists of three layers: Bruch’s membrane, capillary layer, and outer vessel layer. The choroid’s primary job is to feed the retina’s outer layers.
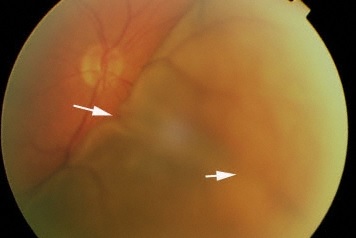
Subretinal folds typically become visible over the peripheral retina of the eye, this clinical feature is known as the choroidal fold. Choroidal Folds are frequently parallel and horizontal, although they can also be vertical, oblique, and irregular. In terms of length and width, these folds represent the choroid’s undulations, as well as those of the retinal pigment epithelium and the underlying neurosensory retina.
Nettleship et al. first defined them clinically as choroidal folds, but Gass renamed them chorioretinal folds to reflect the complete pathology observed clinically. They are linked to ocular and orbital problems.
Choroidal Folds Symptoms
Choroidal folds may not cause any symptoms at all, depending on where they are located and when they first appear, they may cause metamorphopsia and a reduction in vision. When the folds include the macula, they can decrease visual acuity either directly or indirectly, typically by acute deformation of the overlaying retinal photoreceptors, choroidal fold-related maculopathy, or when accompanied by retinal illness.
A hyperopic shift in one’s refractive error causes a painless loss of vision in those with acquired hyperopia with choroidal folds syndrome, although, with more hyperopic correction, visual acuity usually returns to normal levels.
Choroidal Folds Causes
Choroidal folds are not a sign of a specific disease. Instead, they are caused by biomechanical stresses in the choroid. A thicker choroid or a posterior flattening of the globe due to scleral compression or thickening may be the source of these strains.
Some of the common causes of Choroidal Folds are as follows:
- Hypotony
- Posterior Scleritis
- Intracranial Hypertension
- Choroidal Neovascularization
- Injury or Shock
- Eye Surgery
- Acquired Hyperopia
Choroidal Folds Diagnosis
Patients who have no symptoms or are having routine ophthalmological exams for other conditions are frequently found to have Choroidal Folds. CRFs may produce metamorphopsia, photopsia, or visual abnormalities, leading patients to ophthalmologists.
Choroidal Folds typically manifest during a fundoscopic examination as parallel, alternating dark and yellow lines. They are placed horizontally, obliquely, vertically, and concentrically.
Fundus fluorescein angiography, often known as FA, is regarded as one of the imaging methods with the highest degree of sensitivity for the diagnosis of Choroidal Folds. To arrive at an accurate diagnosis, it is preferred to perform imaging scans of the orbits and brain using ultrasonography, computed tomography (CT), or magnetic resonance (MR).
Choroidal Folds Treatment
Choroidal folds are an uncommon sign that can be seen in the back of the eye. Perhaps though they are uncommon, it is essential to recognize them because of the possibility that they are associated with pathological disorders that pose a risk to the patient’s vision or even their lives.
Compared to bilateral presentations, unilateral patients of choroidal folds are more likely to develop orbital illness and more serious ocular disease. It is difficult to diagnose the pathologic conditions that caused the choroidal folds. For potentially serious illnesses to be diagnosed with optimal investigations, a correct approach that is adapted to the specific aspects of each case is important.
Idiopathic patients can be identified since they are typically asymptomatic. In most cases of acquired hyperopia, no therapy is required, and the condition can simply be observed. Treatment for choroidal tumors varies widely based on the type of tumor that is suspected.
Most of the time choroidal folds are treated with observation combined with a lifestyle adjustment. Argon laser, green 532 nm frequency-doubled Nd-YAG laser photocoagulation, or micropulse diode laser to the point of leakage are all used to treat chronic or recurrent instances. Another treatment option is photodynamic therapy. Anti-corticosteroid treatment and carbonic anhydrase inhibitors are also attempted, with varying degrees of success.
 Health & Care Information
Health & Care Information