stercoral colitis is an inflammation in the colonic wall, which increases Luminal Distention (A painful sensation followed by bloating, which leads to secondary motility changes in severe conditions) and mechanical pressure on the colonic wall, resulting from holding hard fecal material for a long time. stercoral colitis is common in patients with chronic constipation because chronic constipation leads to the development of large, hard, and dry stool, which can build up pressure on the intestinal walls and cause ulcers leading to chronic perforation.
As a result of a dilated colon and stretching, the intestinal wall becomes thin. The blood supply to this area decreases as the intraluminal stretching and higher pressure on the intestinal wall increases. In the case of stercoral colitis and colonic perforation, there is a 35% mortality rate.
The condition of Stercoral colitis was reported in 1894, for the first time.
What is Stercoral Colitis?
Stercoral colitis is inflammatory colitis caused by increased intraluminal pressure due to damaged fecal material in the colon segments. Stercoral colitis can range from diseased fecal matter associated with inflammation to colon perforation. SC’s most important complication is colon perforation, which is reported to be associated with a mortality rate of 32–57%.
Increased pressure due to holding of hard and dry fecal matter for a long time may cause ulceration, which may lead to perforation if left untreated.
Stercoral Colitis Symptoms
It occurs primarily in elderly patients (often bedridden due to dementia, stroke, or orthopedic surgery). Less commonly, it can also be seen in younger patients who have metabolic, neurological, and / or muscle disorders that cause constipation.
The symptoms of Stercoral Colitis include;
● The patient may have a medical history of chronic constipation.
● The patient may be asymptomatic.
● The patient may have only mild abdominal pain at the initial stages.
● The patient may have abdominal pain or abdominal tenderness.
● The patient may experience vomiting and distention.
● The patient may experience mood swings.
● Bowel obstruction is also seen in the patients of Stercoral colitis.
● Painful hemorrhoids may also be seen.
● The patient may have symptoms of hypothyroidism.
● Constipation is the symptom experienced in the early stages of Stercoral colitis.
Stercoral Colitis Causes
Patients with stercoral colitis almost always have chronic constipation, comorbidities, and advanced age, which can contribute to life-threatening complications. Chronic constipation, aggravated by physical inactivity, leads to a vicious cycle of constipation leading to more severe stool blockage and blockage leading to blockage of colon movement.
Comorbid neurologic and psychiatric disorders may delay the diagnosis of Stercoral Colitis due to poor history and physical examination. The lack of definitive clinical data on KS makes imaging-based diagnosis important. Late diagnosis of this disease can lead to severe complications and even death.
So the main causes of Stercoral Colitis are;
● Constipation
● Lack of exercise
● Improper diet
● Lack of fiber components in diet
● Poor water intake
● Hypothyroidism
● Hernia
● Tumor
● Painful Hemorrhoids
● Hypomagnesia
● Lack of sleep which may lead to poor metabolism and, ultimately, constipation
● Hypercalcemia
● Volvulus
● Malignant Bowel Obstruction
Stercoral Colitis Treatment
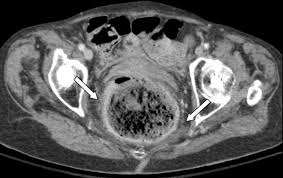
Steric colitis can be fatal and requires immediate treatment. The importance of early recognition is very high to avoid complications associated with late diagnosis. Early diagnosis by computed tomography (CT) demonstrates fecaloma, focal thickening of the dilated sigmoid and rectal wall representing edema due to ischemia or ulceration, and peri-suture or perirectal fat. Most often, the lesion occurs in the sigmoid and rectosigmoid colon, which, in addition to the relatively poor blood supply, have the narrowest diameter of the colon, which provides a higher intraluminal pressure.
Once the diagnosis is made, the patient should be treated appropriately and promptly to avoid morbidity and mortality from bowel perforation and peritonitis. Non-surgical bowel management, enemas, manual removal of feces by rectal examination, or endoscopy are considered the standard of care. However, endoscopically guided disinfection is considered the standard of care. Surgical treatment is intended for patients with signs of peritonitis caused by perforation of the colon wall and includes surgical resection of the enlarged colon.
Therefore, early diagnosis and treatment with bowel cleansing and stool disinfection are necessary to avoid the fatal consequences of this condition. This early assessment is performed with CT findings with focal thickening of the colon wall, curling of pericolic fat in the segment showing fecal blockage, and the presence of extraluminal gas bubbles or abscess.
Contacting a doctor is very necessary if you develop any of the above-mentioned symptoms. This may be treated nonsurgically if there is no proof of bowel perforation or ischemia.
 Health & Care Information
Health & Care Information