Learn all about congenital neutropenia definition, causes, prognosis, life span, treatment. Congenital neutropenia is characterized by chronic neutropenia due to a constitutional genetic defect. Since the early 1990s, and particularly during the last decade, the molecular bases of several entities have been discovered, leading to changes in the disease classification.
Severe congenital neutropenia is a condition that causes affected individuals to be prone to recurrent infections The Kostmann’s form of this disorder is very rare; it is caused by disabling mutations in the HAXl gene, which encodes HAX1, a mitochondrial protein that inhibits apoptosis. There are also autosomal dominant and sporadic forms of severe congenital neutropenia that are caused by mutations in the ELA2 gene, which encodes the serine protease neutrophil elastase
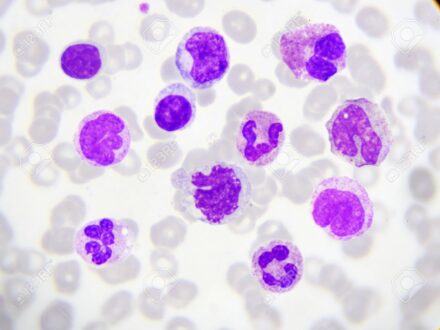
There are several forms of congenital neutropenia varying in the severity of reduction of neutrophil counts and the associated clinical problems. In one severe form, congenital agranulocytosis or Kostmann’s syndrome, neutrophils are severely reduced from birth, often to less than 0.1 x 109/L. There is often a mild increase in blood monocytes and blood and marrow eosinophils, but the reasons for this observation are not known.
The increase may be due to higher levels of endogenous haematopoietic growth factors during chronic inflammation, or because production of blood cells is diverted away from the neutrophil lineae. Neutrophil counts are always quiet low, but in some patients, in response to severe illness and infection, slightly higher counts may be observed
Congenital neutropenia comprises a variety of genetically heterogeneous phenotypic traits. Molecular elucidation of the underlying genetic defects has yielded important insights into the physiology of neutrophil differentiation and function. Non-syndromic variants of congenital neutropenia are caused by mutations in ELA2, HAX1, GFI1, or WAS.
What is Congenital Neutropenia?
The term congenital neutropenia encompasses a family of neutropenic disorders, both permanent and intermittent,. s a rare blood disorder characterized by abnormally low levels of certain white blood cells (neutrophils) in the body (neutropenia). Neutrophils play an essential role in fighting bacterial infections by surrounding and destroying invading bacteria (phagocytosis).
Congenital Neutropenia Definition
Congenital neutropenia is defined as the lack of neutrophils a type of white blood cell that is an essential first line of defense against infections. The main complication of neutropenia is an increased risk of infection. Congenital neutropenia is defined as an absolute neutrophil count (ANC) of less than 1500 per microliter (1500/microL) at the birth; severe neutropenia is defined as an ANC of less than 500/microL.
Congenital Neutropenia Causes
Congenital neutropenia is caused by various reasons. Premature babies are more likely to be born with neutropenia than babies born near their due date. The condition affects 6 to 8 percent of newborns in neonatal intensive care units. As a general rule, the smaller the baby, the more likely they are to have neutropenia.
- Certain medications, including antibiotics and drugs for high blood pressure, psychiatric disorders, and epilepsy.
- Barth syndrome, a genetic disorder affecting multiple systems
- myelodysplastic syndromes, which are a group of disorders characterized by dysfunctional blood cells due to problems with bone marrow production
- myelofibrosis, a rare bone marrow problem, also known as osteomyelofibrosis
- alcohol dependency
- Vitamin deficiencies, most commonly vitamin B12, folate, and copper deficiency.
- Sepsis, an infection of the bloodstream that uses up neutrophils quicker than they can be produced.
- Pearson syndrome
- certain infections, including hepatitis A, B, and C, HIV/AIDS, malaria, tuberculosis, dengue fever, and Lyme disease.
- hypersplenism, or an enlarged spleen
- Some autoimmune conditions can target neutrophils, reducing their number. These conditions include:
- Crohn’s disease
- rheumatoid arthritis
- Lupus.
Congenital Neutropenia Prognosis
The prognosis depends heavily on the quality of care and timeliness of treatment of severe infections, but also on the possibility of a bone marrow transplant, particularly in cases with malignant transformation.
Congenital Neutropenia Life Span
The life expectancy for people with severe congenital neutropenia has improved greatly. With increasing age, you are at increased risk for myelodysplastic syndrome (MDS) and leukemia (mostly acute myeloid leukemia) compared to the general population. This risk was thought to be secondary to G-CSF treatment but appears to be a complication of the condition. Approximately 20 percent of people with severe congenital neutropenia develop certain cancerous conditions of the blood, particularly myelodysplastic syndrome or leukemia during adolescence. These patients’ life expectancy routinely exceeds 30 years.
Congenital Neutropenia Treatment
Congenital neutropenia treatment includes:
- Antibiotics for fever; in neutropenic fever, the assumption is made that there is an infection causing the fever even when the source can’t be found.
- A treatment called granulocyte colony-stimulating factor (G-CSF). This stimulates the bone marrow to produce more white blood cells. It is used for several types of neutropenia, including low white cell count from chemotherapy. This treatment can be lifesaving in these cases.
- Changing medications, if possible, in cases of drug-induced neutropenia
- Granulocyte (white blood cell) transfusion (very uncommon)
- Stem cell transplants may be useful in treating some types of severe neutropenia, including those caused by bone marrow problems.
 Health & Care Information
Health & Care Information